Can we talk about it? The role of occupational therapy in suicide
*Disclaimer – The following contains details about suicide and should be read at the reader’s discretion. This article intends to be informative and educational, when unsure how to proceed, 000 should be called. If the following information and discussion raise any concerns, please contact Lifeline on 13 11 14 or your regular doctor.
Why is mental health and suicide, in particular suicide, still so hard to talk about?
In 2020 3,139 individuals died from suicide, an average of 8.5 people per day – Close to 3 times the 1,110 people who died on our roads that same year. This number grows exponentially to over 65,000 attempts in the same year, and over 33,000 or close to 90 hospitalisations a day due to injuries or overdoses from non-fatal suicides. Keeping in mind these figures don’t include individuals that weren’t hospitalised after attempts, and those experiencing suicidal ideation, the initial figure of 3,139 represents a much larger issue.
With several campaigns including ‘RU OK?’ and ‘The Push-Up Challenge,’ the approach to suicide and reducing the attached stigma has come a long way in recent years. But it still takes courage to ask a friend, a family member, or a work colleague; simply and directly, ‘are you okay?’ What if they are okay? Will they laugh? Or will they be insulted you asked? And how do you respond if things aren’t okay? It’s these very questions that often stop us from saying anything.
Dispelling the myths – What are the actual facts?
False: Most suicides occur without warning.
True: People will often exhibit verbal or behavioural warning signs or display changes in their daily functioning. Some suicides occur without any obvious warning, but it’s important to understand what the warning signs are and look out for them.
False: Once suicidal, always suicidal.
True: Active thoughts of suicide often stem from an acute stressful event that appears unmanageable or can subsequently bring to light deep unresolved emotions or trauma. By recognising and dealing with these events as they arise, as well as addressing the underlying issues, the suicidal ideation will often dissipate. Thoughts of suicide can return but they are rarely permanent.
False: Talking about suicide encourages or leads to suicide.
True: There is still a large amount of stigma associated with suicide and as a result, many people are afraid to speak about it. Evidence suggests that talking about suicide not only reduces the stigma but also allows individuals to seek help, rethink their own opinions and share their stories with others. We all need to talk more about suicide.
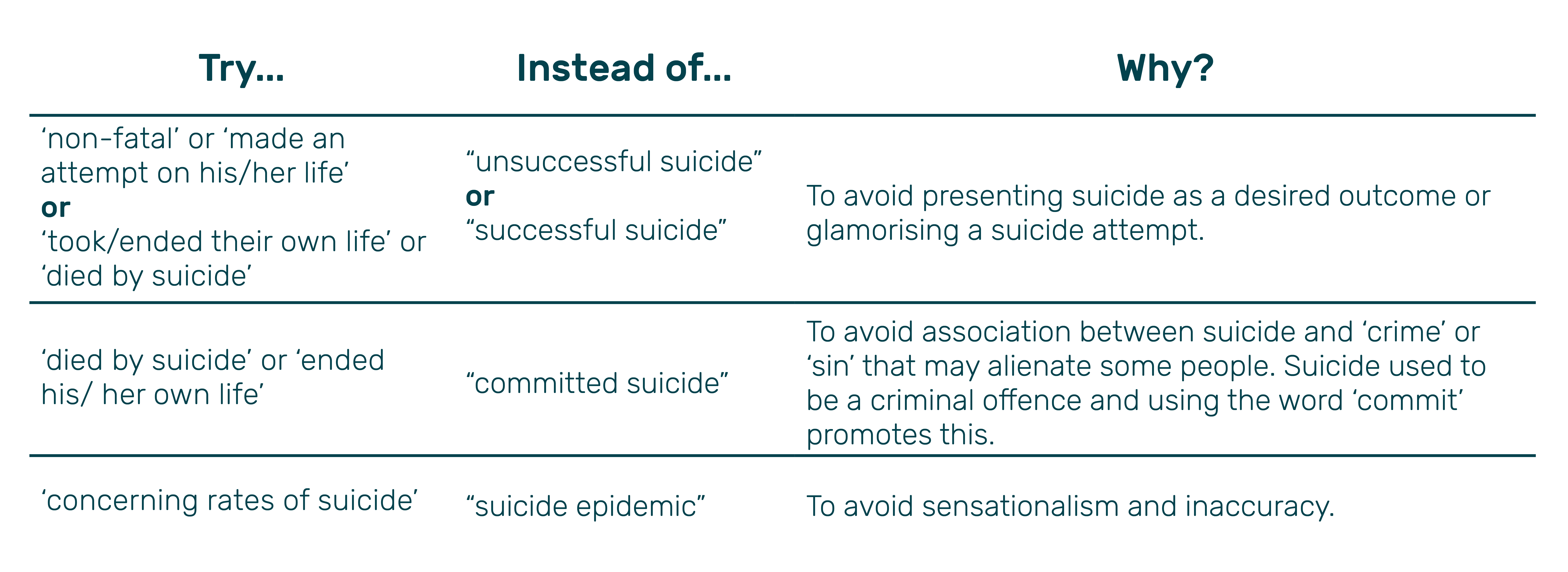
Words hold power
The terminology and descriptions we use when describing something or someone can have a lasting impact on a person’s thoughts and behaviours. As a result, the language we use to discuss suicide can help in reducing the stigma or glamorising the issue and reduce the possibility of alienating those who are impacted. For that reason, and while each person may not agree with all of the below, the following list has been compiled to aid in the discussions you might have (Alberta Mental Health Board, n.d):
The role of Occupational Therapy
Occupational Therapy is a holistic and client-centred profession that at its heart seeks to build and maintain independence and promote participation in meaningful activities (Occupational Therapy Australia, n.d). Occupational engagement gives meaning and provides the purpose and being deprived of engagement can lead to a personal crisis, a loss of identity, an increase in illness symptoms, and environmental challenges. For that reason, the perception is that suicide only falls within the realm of mental illness or with mental health Occupational Therapists/practitioners when in reality it is equally as prevalent in physical health settings.
This puts Occupational Therapists (like at KEO Care) in a key position to identify and intervene at all levels:
- Prevention: Promoting awareness and reducing the stigma of suicide within the wider community. Recognising key issues/concerns in an individual that can lead to suicidal thoughts and behaviours.
- Intervention: Utilising rapport/trust with an individual to address thoughts and plans of suicide and creating a safety plan.
- Postvention: Rebuilding a sense of purpose and engagement in occupations and community.
The Push Up Challenge
KEO Care has signed up to complete The Push for Better Foundations ‘The Push-Up challenge’ over the month of June. ‘The Push Up Challenge’ requires participants to complete 3,139 push-ups or a similar physical challenge within a team or solo, representing each of the individual lives lost to suicide in 2020.
Look out for some pictures and videos of some of the 25 employees registered to complete the challenge!
Head to Health
Head to Health, provided by the Australian Department of Health brings together apps, online programs, online forums and phone services as well as a range of digital information resources. Whether you are trying to improve your sense of wellbeing, looking for help with something that is bothering you, or helping someone you care about – Head to Health is a good place to start.
Head to Health provides care navigation, access to a multidisciplinary mental health team at Primary Health Network hubs and a team-care approach, to complement and supplement GP care.
You can call 1800 595 212 to speak to the Head to Health intake team, an experienced mental health professional will listen and work with you to find the best way to get the help you need.
Resources and more details are available at: Head to Health
Please note, that Head to Health is not a crisis service and those requiring immediate care or who are at risk of harm to themselves or others call 000.
For urgent support call:
- Lifeline 13 11 14
- SuicideLine 1300 651 251
References
Alberta Mental Health Board. (n.d). What’s in a word? The language of suicide. Retrieved from http://www.albertahealthservices.ca/MentalHealthWellness/hi-mhw-sps-language-of-suicide-1p.pdf
Occupational Therapy Australia. (n.d). About Occupational Therapy. Retrieved from OTAus
About the author
Jarrah Brown is an occupational therapist at KEO Care and is experienced within the mental health space. Jarrah started his career within the non-profit community space before transitioning to KEO Care at the beginning of 2021. To further build on his interest in this area, in particular schizophrenia, Jarrah intends to do additional professional development in delivering a holistic approach to service delivery that emphasises that recovery is possible and is most effective when it is participant centred.
Jarrah has recently taken on the role of Team Leader in one of the multidisciplinary teams. Jarrah is passionate about supporting and empowering each of his team members to find the answers to their questions and then be able to reflect on them.
“We do not learn from experience … we learn from reflecting on experience” – John Dewey.
